Clinician burnout is an issue that gets a lot of attention in medicine these days, and with good reason. In a recent study, 49 percent of physicians reported being burned out, with those practicing emergency medicine feeling it the most. Clinicians aren’t the only ones in the hospital who are suffering the workplace blues, however.
CEOs and healthcare leaders are leaving medicine because of burnout at a much higher rate than other team members. One study found that 70% of leadership turnover was due to burnout—compared with 40% for staff in general. Another study concluded that 74 percent of healthcare leaders admitted to having felt burned out within the prior six months, 93 percent believe that burnout is negatively affecting their organization, and 47 percent are less hopeful about the future of healthcare leadership.
WHAT'S CAUSING THESE LEVELS OF FRUSTRATION?
We’ve identified four key issues facing healthcare CEOs that significantly contribute to burnout. See how they are negatively affecting the satisfaction of leaders and what can be done to mitigate them.
STAFF TURNOVER AND RETENTION
It’s no surprise when almost half the workforce are reporting burnout that turnover follows as a result. Clinicians and hospital staff are leaving their jobs for what they hope are greener pastures—or leaving healthcare altogether.
Healthcare leaders can lessen staff turnover and increase worker satisfaction by starting with one of the primary causes of frustration–outdated, rigid, difficult to use EHRs. In fact, 75 percent of those reporting burnout cited the EHR as a source. Unnecessary clicks, manual entry of information, duplicative tasks and clunky workflows all contribute to the dissatisfaction.
The right EHR, however, saves time for clinicians through automation of tasks, streamlining of reporting, and an intuitive interface that makes it easy to see where and when to document patient information. It should empower the user by allowing them to create, customize, and manage their own workflows so they work the way clinicians need them to. It should provide helpful tools that make every shift easier and the delivery of care more efficient.
FINANCIAL PRESSURE
It has been well publicized that many healthcare organizations are operating with razor thin profit margins. This is fueled by skyrocketing labor costs, economy-wide inflation, significant underpayment, delays in posting charges, and health insurer practices like prior authorizations and denials. This can be further exacerbated by harmful incidents such as non-compliance and cybersecurity attacks–including ransomware.
Your EHR should help battle these financial pressures by ensuring accuracy through its documentation, and reporting, minimizing audit and reimbursement issues. Facility led configuration that allows you to customize charge codes, descriptions, departments, rates, and more makes billing more efficient and less likely to be incomplete. A low/no code design that prevents vendor lock-in can help you avoid paying third party fees.
As mentioned above, staff turnover is a major concern that can lead to the additional costs of recruiting, hiring, and training new staff members. An EHR that minimizes staff turnover through user satisfaction can help keep those costs down by helping you retain your staff.
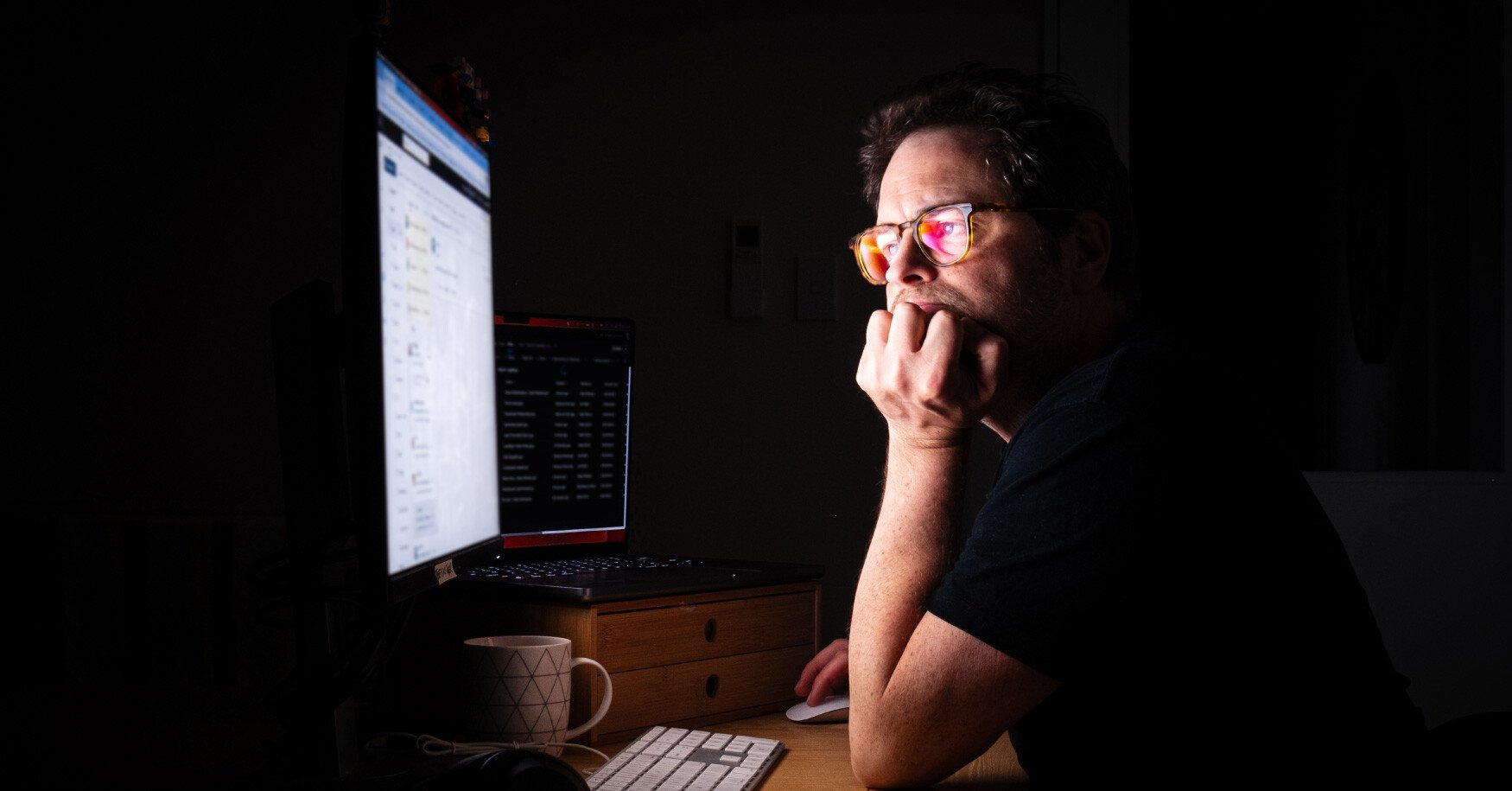
WORK/LIFE BALANCE
CEOs have a lot on their plate. They’re constantly pulled in different directions, with a multitude of stakeholders to satisfy. Even the best multitaskers can only do so much and it’s impossible to be at two places at once. This leads to healthcare leaders working long hours–often during nights and weekends.
An EHR should help address this by enhancing communication, which reduces CEO involvement in team coordination. It should enable timely incident management and follow up, minimizing CEO intervention. If your EHR is fully compliant with industry and government regulations, audit time can be reduced, and an EHR that facilitates higher-quality care reduces the frequency of involvement in operational oversight. Lastly, medication adherence and patient engagement tools reduce readmissions, saving time on corrective actions.
DROP IN QUALITY MEASURES
When quality measures drop, the pressure on healthcare leaders rises. Hospital CEOs are directly responsible for how their facilities perform. Poor results in key metrics such as patient satisfaction, care quality, readmission rates, and clinical outcomes can severely impact a hospital’s reputation, financial stability, and government oversight.
With an EHR that closely tracks performance and alerts the CEO of any issues related to care quality in a timely manner, these problems can be addressed before they become catastrophes. An EHR’s Clinical Decision Support should ensure quality measures are being met in real time to prevent mistakes and promote thoroughness. Flowsheets should be configured by facility, department, and role to support familiar workflows, leading to less errors.
MEET THE EHR THAT WILL LET YOU REST EASY
Managing burnout is crucial at every level of your organization. With a modern, user-friendly solution like Juno EHR, you can lessen the individual factors that contribute to the collective stress CEOs are currently facing. We’d love to show you how Juno EHR can alleviate many of your concerns.